Prostate cancer (PCa) is the second most frequent malignancy in men worldwide, accounting for 1,414,259 new cases and causing around 3.8% of all deaths from cancer in men in 20201. Despite its prevalence, PCa diagnosis is far from ideal. It usually requires a transrectal ultrasound-guided (TRUS) biopsy, a painful procedure with potential side-effects2, including sampling errors, overdetection of indolent PCa, and misclassification3.
This is where a virtual biopsy approach powered by MRI comes into play, offering a non-invasive, precise alternative that could revolutionize prostate cancer detection and diagnosis.
What is MRI in prostate cancer detection?
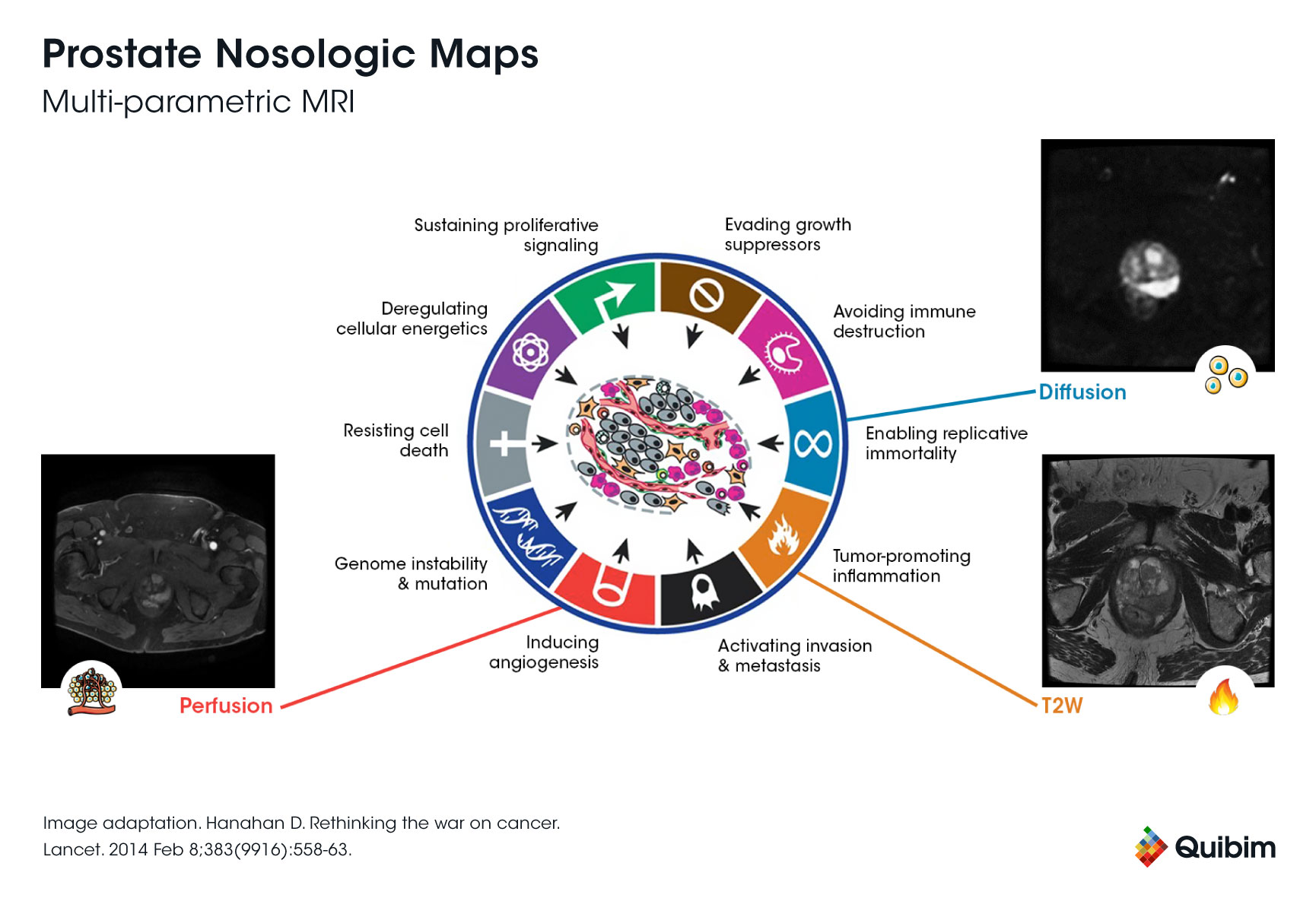
Multiparametric magnetic resonance imaging (mpMRI) provides a better visualization of the entire prostate gland in a completely non-invasive way. This makes it a promising tool for virtual biopsy prostate applications. By identifying the most suspicious areas in the prostate gland, mpMRI helps physicians target specific regions during biopsies, reducing the need for random sampling.
At present, clinical evidence increasingly supports the use of mpMRI as a pre-biopsy step, enhancing diagnostic accuracy4,5, and offering a pathway to cirtual MRI diagnostics6,7. However, the population-wide adoption of mpMRI still needs to overcome some hurdles.
On the one hand, since it may clearly change the PCa pathway, a sharp increase in the number of men who will undergo prostate MRI is expected. Providing good image quality and diagnostic accuracy while meeting the demands of the expected high workload will be challenging.
On the other hand, from a clinical point of view, the greatest concern arises from its highly variable accuracy across institutions and among individual radiologists8. Despite the implementation of a standardized reporting system such as the Prostate Imaging Reporting and Data System (PI-RADS)9, there is still room for improvement in mpMRI reporting.
Finally, and as discussed by the American Urologists Association (AUA), there are several significant impediments to the adoption of mpMRI as a stand-alone, population-based screening strategy, so it seems that there is still a long way to go before MRI scales up as a standard-of-care screening tool, as mammography did in breast cancer. However, advances in AI and radiomics may accelerate the adoption of MRI as a reliable virtual biopsy method.
Could artificial intelligence (AI) help to create more reliable and faster MRI scans speeding up this process?
Artificial intelligence: Boosting the power of MRI
AI is a rapidly emerging technology and has gained massive interest in medical imaging research, mainly in a preclinical setting10. By combining radiomics and machine learning, AI enhances the diagnostic capabilities of MRI, potentially positioning it as a reliable virtual biopsy prostate solution.
Several studies have evaluated the performance of computer-aided diagnosis (CAD) coupled with radiomics and machine learning to diagnose PCa from clinical images with promising results11. Recently, the group led by Nickolas Papanikolaou at the Champalimaud Foundation in Lisbon, Portugal, has provided new insights into the prediction of PCa disease aggressiveness using MRI radiomics, a methodology that enables to transform medical images into high dimension mineable data12.
Thus, based on the hypothesis that tumor tissue characteristics can be quantified by radiomic features extracted from bi-parametric MRI (a shorter type of MRI scan that uses the same device to image the prostate to detect signs of cancer), the investigators developed different supervised machine learning models to predict biological aggressiveness. Their results demonstrated that MRI-based radiomic features allowed the identification of clinically significant PCa. Also, they observed that radiomic features extracted from the whole prostate gland produced better models than those extracted from specific regions, highlighting the relevance of those areas surrounding the tumor lesions as important sources of information.
Interestingly, AI does not only have the potential to improve diagnosis but can also be useful in metastasis detection and prediction of response to treatment, paving the way for broader applications of virtual MRI technology in oncology. Indeed, those are some of the aims of ProCAncer-I, a project led by Dr. Papanikolau among others, that brings together 20 partners, including PCa centers of reference, world leaders in AI, and innovative small and medium-sized enterprises (https://www.procancer-i.eu/) and that aspires to create the largest interoperable, high-quality mpMRI dataset worldwide/globally (currently including >17,000 cases).
Quibim is proud to lead tasks within key work packages of this ambitious initiative, including image and data annotation-related activities, and the implementation of monitoring, logging, and retraining of AI models.
The potential of virtual biopsies in other organs
While prostate cancer remains a key focus, the concept of a virtual biopsy extends to other organs, including breast and liver.
Virtual biopsy for breast cancer
MRI has long been a cornerstone in breast cancer diagnostics. With advancements in AI and radiomics, MRI is becoming a potential tool for virtual biopsy breast applications. This approach can help identify malignancies and guide treatment plans without the need for invasive tissue sampling.
Virtual biopsy for liver disease
In the field of hepatology, MRI-based virtual biopsy liver methods are gaining traction. These techniques provide critical insights into liver health, including fibrosis, steatosis, and tumor detection, reducing the need for traditional biopsies.
The road ahead for AI-Driven virtual biopsies
Although AI-enhanced virtual biopsy technology is not yet ready for widespread clinical deployment, its potential is undeniable. By addressing current limitations in conventional biopsies and mpMRI, AI-driven solutions will likely redefine cancer diagnostics across various medical fields.
Quibim remains at the forefront of these innovations, contributing to cutting-edge research and collaborations aimed at unlocking the full potential of virtual biopsies.
The integration of advanced MRI techniques and AI-driven solutions marks a significant leap towards making virtual biopsy a reality. Whether for prostate, breast, or liver diagnostics, this approach promises a future where invasive procedures become the exception rather than the norm.
As technology continues to evolve, the role of virtual MRI in cancer detection and management will undoubtedly expand, improving outcomes and enhancing the standard of care for patients worldwide.
References
- Observatory., G.C. Cancer Fact Sheets; prostate cancer. [cited 2022 March]; Available from: https://gco.iarc.fr/today/data/factsheets/cancers/27-Prostate-fact-sheet.pdf.
- Loeb, S., et al., Systematic review of complications of prostate biopsy. Eur Urol, 2013. 64(6): p. 876-92.
- Pokorny, M.R., et al., Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol, 2014. 66(1): p. 22-9.
- Haffner, J., et al., Role of magnetic resonance imaging before initial biopsy: comparison of magnetic resonance imaging-targeted and systematic biopsy for significant prostate cancer detection. BJU Int, 2011. 108(8 Pt 2): p. E171-8.
- Kasivisvanathan, V., et al., MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med, 2018. 378(19): p. 1767-1777.
- American Urological Association (AUA). Standard operating procedure for multiparametric magnetic resonance imaging in the diagnosis, staging and management of prostate cancer. [cited 2022 March]; Available from: https://www.auanet.org/guidelines/guidelines/mri-of-the-prostate-sop.
- European Association of Urologists (EAU). Guidelines on prostate cancer. [cited 2022 March]; Available from: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-EANM-ESTRO-ESUR-ISUP_SIOG-Guidelines-on-Prostate-Cancer-2022.pdf.
- Tosoian, J.J., Awaiting the perfect diagnostic test: optimal prostate cancer care begins without a diagnosis. Prostate Cancer Prostatic Dis, 2022.
- Stabile, A., et al., Multiparametric MRI for prostate cancer diagnosis: current status and future directions. Nat Rev Urol, 2020. 17(1): p. 41-61.
- European Association of Urologists (EAU). EAU Congress 22. Risk stratification and artificial intelligence in MRI-based early detection of prostate cancer. [cited 2022 March]; Available from: https://eaucongress.uroweb.org/risk-stratification-and-artificial-intelligence-in-mri-based-early-detection-of-prostate-cancer/.
- Van Booven, D.J., et al., A Systematic Review of Artificial Intelligence in Prostate Cancer. Res Rep Urol, 2021. 13: p. 31-39.
- Van Timmeren, J.E., et al., Radiomics in medical imaging-“how-to” guide and critical reflection. Insights Imaging, 2020. 11(1): p. 91.
