The challenge
B-cell lymphoma patients who relapse after two lines of treatment are candidates for chimeric antigen receptor T cell (CAR-T) therapy, which has shown notable success with complete remission rates ranging from 40% to 54%.
However, despite these advancements, a significant proportion of patients progress or relapse after CAR-T infusion. Additionally, CAR-T therapy can lead to serious side effects such as immune effector cell-associated neurotoxicity syndrome (ICANS). Traditional clinical predictors alone have been insufficient to accurately predict patient outcomes, highlighting the need for identifying non-invasive biomarkers that may allow better patient risk stratification and management.
The solution
In this multicentric retrospective study, Quibim developed advanced imaging-based prognostic and predictive models using logistic regression and Cox proportional-hazards models to predict CAR-T therapy response at 3 and 6 months, overall survival (OS), progression-free survival (PFS), and the occurrence of ICANS.
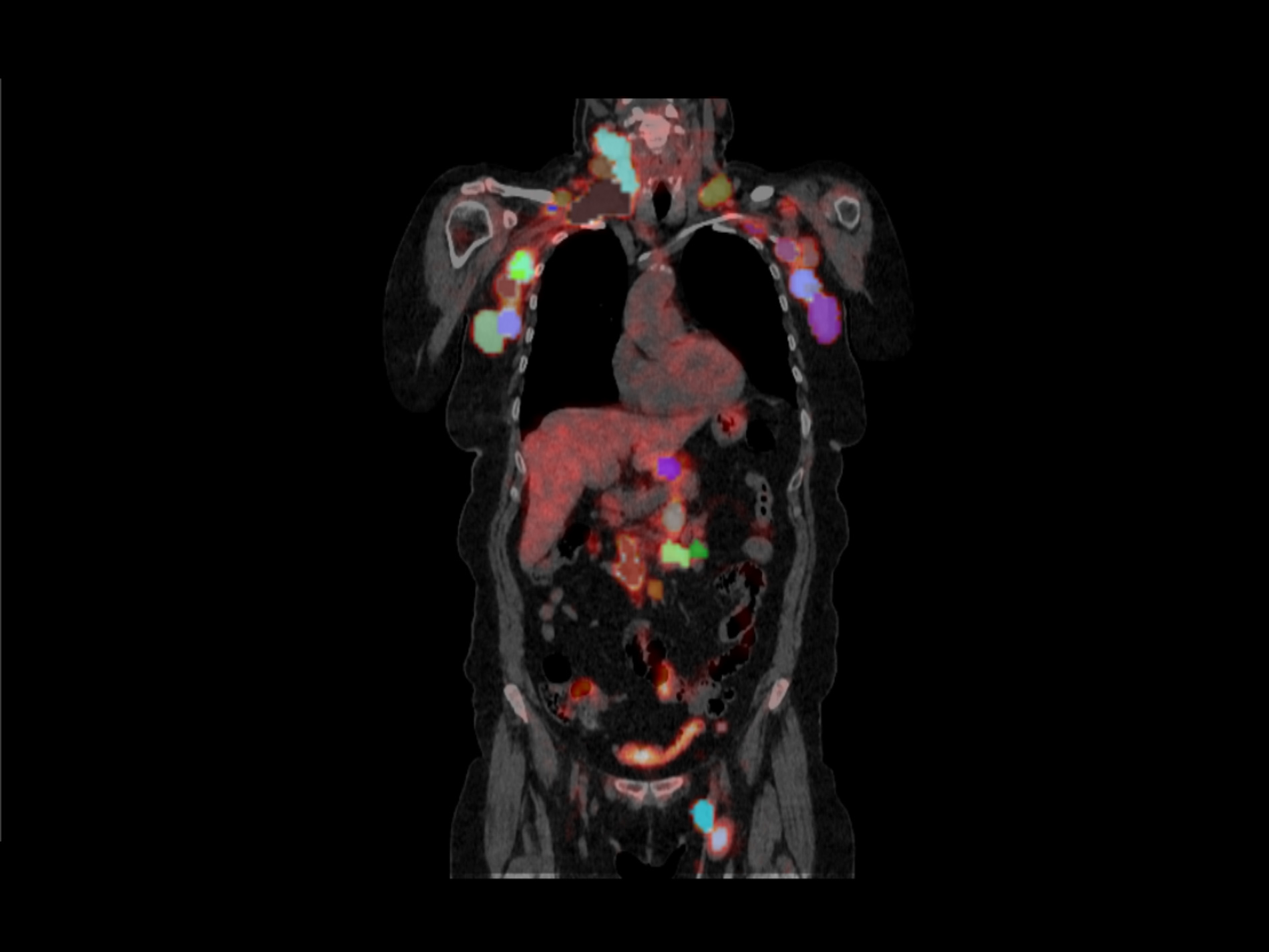
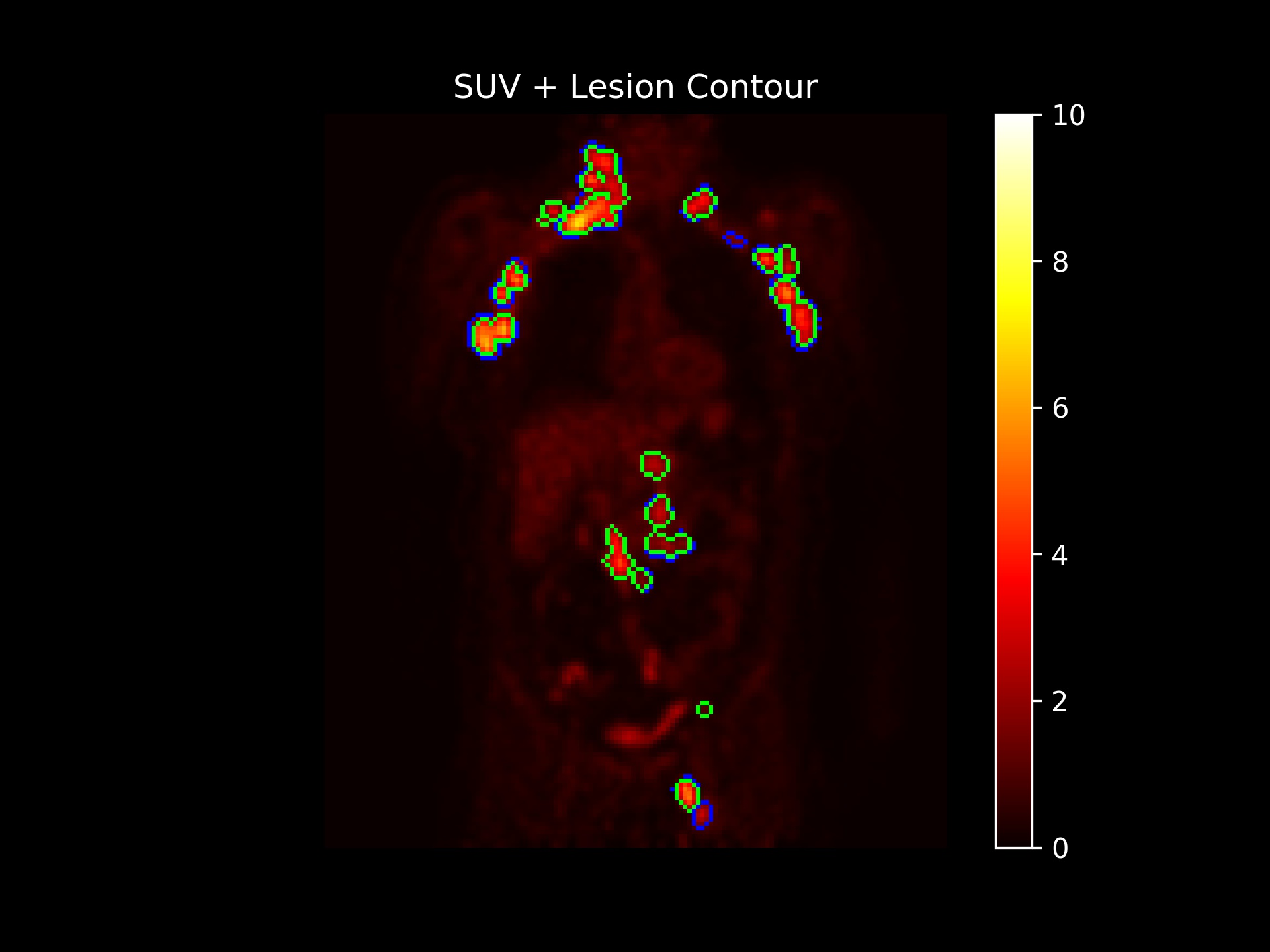
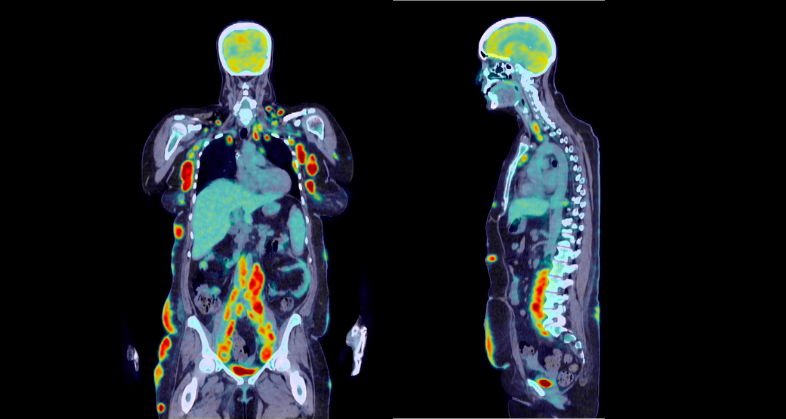
Sixty-five relapsed/refractory (R/R) B-cell lymphoma patients treated with CAR-T cells were included. All visible lesions from pre-treatment 18F-FDG PET/CT scans were segmented, and quantitative imaging features were extracted using the QP-Insights® platform. Quantitative imaging features were combined with relevant clinical variables to develop prognostic and predictive models.
The outcome
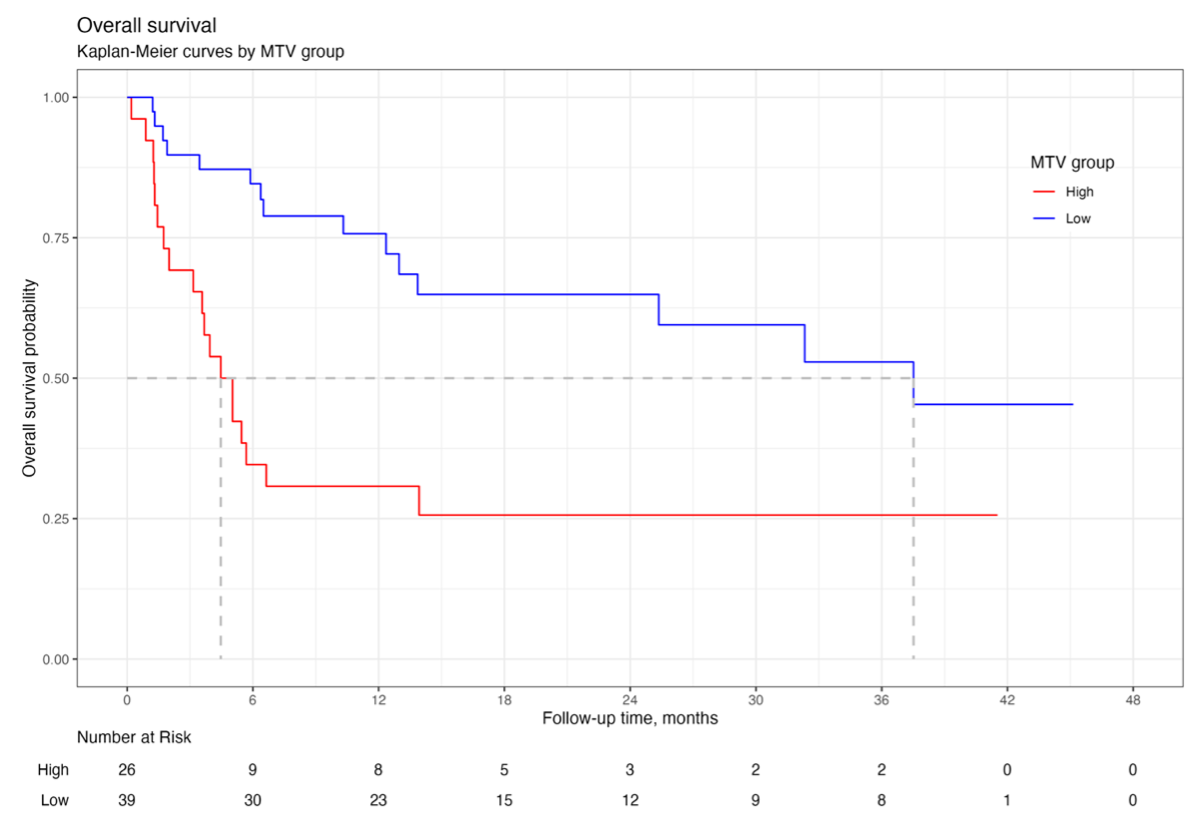
The combined models significantly improved prediction accuracy compared to clinical or imaging features alone. For instance, the model for predicting ICANS achieved an area under the curve (AUC) of 0.830, and those for CAR-T response at 3 and 6 months showed AUCs of 0.754 and 0.818, respectively. Furthermore, the identified total metabolic tumor volume (MTVtotal) cut-off values effectively stratified patients by OS and PFS, with low MTVtotal associated with longer survival times.
These multi-omic models provide a promising tool for risk stratification and personalized treatment, potentially improving outcomes for CAR-T treated R/R B-cell lymphoma patients and addressing current unmet needs in designing clinical trials for CAR-T therapy in which the prediction of side effects can improve the screening process.
Reference
Ferrer-Lores, B., Ortiz-Algarra, A., Picó-Peris, A. et al. Predicting survival, neurotoxicity and response in B-cell lymphoma patients treated with CAR-T therapy using an imaging features-based model. EJNMMI Res 14, 113 (2024).
Related case studies
-
Prognostic value of genetic alterations and 18F-FDG PET/CT imaging features in diffuse large B cell lymphoma
Read more
-
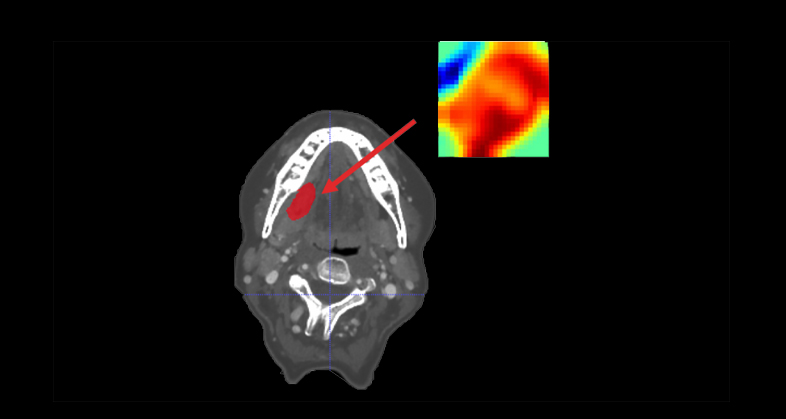
CT-based clinical-radiomics model to predict progression and drive clinical applicability in locally advanced head and neck cancer
Read more
-
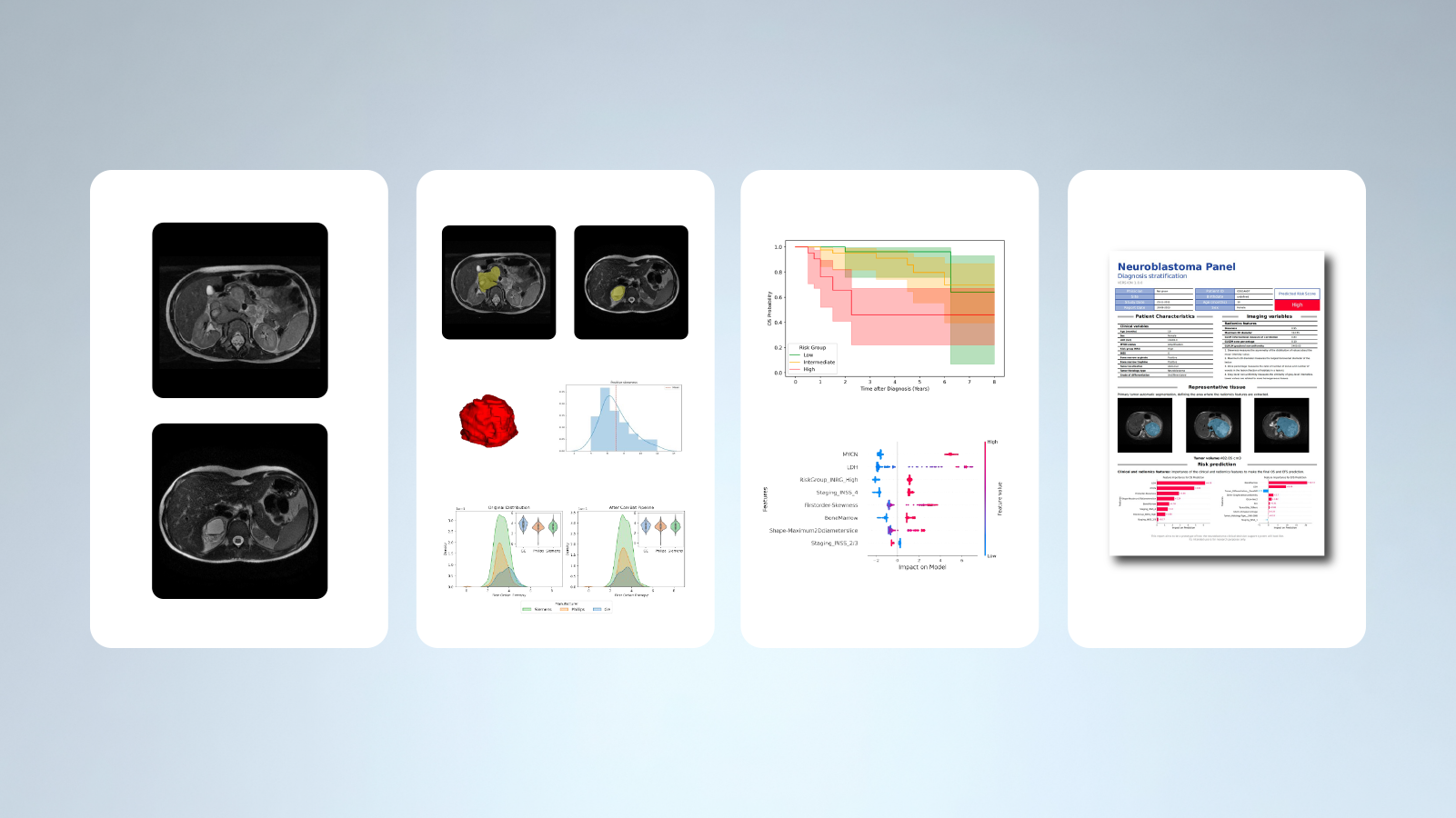
Empowering neuroblastoma risk stratification through AI algorithms
Read more
